Imagine stepping on a scale and seeing a “healthy” number—but what if that figure hides more than it reveals? Body composition changes with time, and age-specific health tools can offer deeper insights than generic measurements. This is where understanding your body mass index (BMI) through a tailored lens becomes critical.
We often hear about body mass index as a standard health indicator, but its interpretation isn’t static. For example, muscle mass in athletes or natural shifts in body fat distribution with age can skew results. That’s why organizations like the Centers for Disease Control and Prevention emphasize using age-adjusted charts for accurate assessments.
These tools help contextualize numbers by comparing them to population data matched to your life stage. For children and teens, growth patterns and sex-specific percentiles matter. Adults, however, focus more on height-weight ratios while acknowledging limitations like not accounting for visceral fat or bone density.
Key Takeaways
- Body mass index charts vary by age to reflect physiological changes
- Muscle mass and body composition impact BMI accuracy
- CDC guidelines provide age-specific percentile ranges for youth
- NIH research highlights BMI’s role in predicting health risks
- Combining BMI with other metrics offers a holistic health picture
While no single metric defines wellness, learning to interpret these charts empowers better conversations with healthcare providers. Let’s explore how to use them effectively—and when to look beyond the numbers.
Introduction: Understanding BMI and Age-Related Health
Health assessments evolve as we do—what worked at 25 might miss critical details at 55. This reality reshapes how we view screening tools like body mass index. While it calculates weight relative to height, health status depends on more than simple math.
Overview of Body Mass Index
The index categorizes individuals into underweight, normal, overweight, or obese ranges. These labels help flag potential health concerns but don’t distinguish muscle from fat. A healthy weight for a 20-year-old athlete might differ from a 60-year-old with similar measurements.
Health authorities use these ranges as initial screens, not final diagnoses. For example, older adults naturally lose muscle mass, which can skew results toward higher BMI categories despite lower body fat.
Why Age Matters in Health Assessment
Children’s growth spurts and hormonal shifts demand different benchmarks than adults. Teens might show temporary spikes without health risks, while middle-aged adults face metabolic changes affecting body composition.
Relying solely on this metric overlooks visceral fat or bone density variations. Combining it with waist measurements or activity levels paints a clearer picture of health status. Recent studies confirm that age-adjusted evaluations better predict cardiovascular risks than generic charts.
Understanding these nuances helps identify health issues early. It also prevents mislabeling active seniors or muscular individuals as high-risk based on outdated standards.
BMI Chart by Age: A Comprehensive Health Tool
Health insights aren’t one-size-fits-all. Tools that adapt to your life stage provide clearer guidance than generic numbers. Let’s break down how to use these resources effectively.
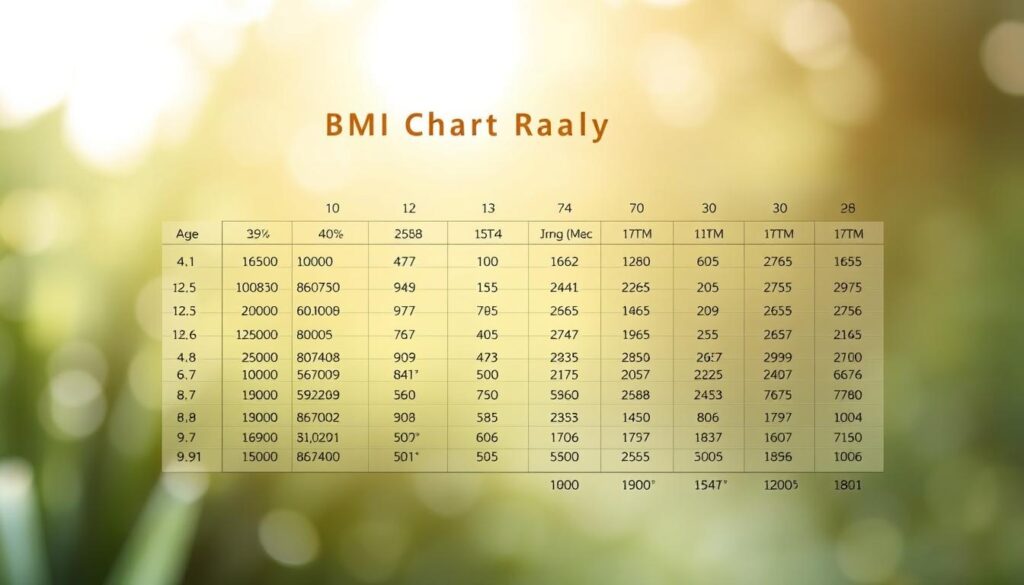
How to Read the BMI Chart by Age
Start by locating your body weight and height on the chart. Match these to your age group’s column—this accounts for natural changes in muscle and fat distribution. The National Heart, Lung, and Blood Institute provides color-coded zones indicating underweight, normal, and overweight ranges.
For adults, focus on the 18.5–24.9 range as a healthy BMI benchmark. Older adults might fall slightly higher without increased risk. Always cross-check with waist circumference measurements—40+ inches (men) or 35+ inches (women) suggests excess abdominal fat.
| Age Group | BMI Range | Additional Metrics |
|---|---|---|
| 20-39 | 18.5–24.9 | Body fat % |
| 40-59 | 23–27.9 | Waist-to-hip ratio |
| 60+ | 25–29.9 | Muscle mass assessment |
Integrating BMI with Other Health Factors
The Centers for Disease Control recommends pairing BMI data with blood pressure and cholesterol levels. For those with health conditions like diabetes, these combined metrics better predict complications.
Consider activity levels and diet quality too. A muscular 50-year-old might show a higher index but have low visceral fat. Use national heart association guidelines to contextualize results—their risk calculators incorporate BMI alongside family history and smoking status.
Exploring the Science Behind BMI and Body Composition
Behind every health metric lies a story of biological complexity that numbers alone can’t fully capture. Body composition—the ratio of fat, muscle, and other tissues—plays a critical role in interpreting screening tools like body mass index.
What BMI Really Measures
This metric calculates weight relative to height squared, offering a quick snapshot of potential health risks. Originally designed for population studies, it’s now used as an initial screening tool. The Centers for Disease Control and Prevention notes it effectively identifies trends but doesn’t differentiate between muscle density and fat storage patterns.
Limitations and Considerations Beyond BMI
Active individuals often face misclassification—a 2023 study found 30% of athletes labeled “overweight” despite low body fat. Older adults may show normal ranges while losing muscle mass, a condition called sarcopenia. Researchers emphasize combining measurements like:
- Waist circumference for visceral fat assessment
- Bioelectrical impedance for muscle-to-fat ratios
- Blood pressure and cholesterol levels
These additions create a clearer health profile, especially for those with unique body types. As one National Institutes of Health report states: “No single metric captures the full spectrum of metabolic wellness.”
Complementary Health Metrics for a Complete Picture
Numbers rarely tell the full story of human health. While body mass index provides a starting point, combining it with other measurements reveals what’s happening beneath the surface. Let’s explore tools that work alongside traditional metrics to assess risk and wellness more accurately.
Waist Circumference and Waist-to-Hip Ratio
Where your body stores fat matters more than total weight. Excess abdominal fat raises health risks like heart disease and diabetes, even with a normal index. The National Institutes of Health recommends measuring waist circumference annually for adults.
Follow these steps for accuracy:
- Stand straight and exhale normally
- Wrap a tape measure around your bare waist
- Record the number just above your hip bones
A waist-to-hip ratio below 0.9 (men) or 0.85 (women) suggests lower metabolic risk. Studies show this measurement predicts cardiovascular issues better than weight alone in older populations.
| Sex | Healthy Waist Circumference | Increased Risk Threshold |
|---|---|---|
| Male | Under 40 inches | 40+ inches |
| Female | Under 35 inches | 35+ inches |
Assessing Muscle Mass and Body Fat Percentage
Muscle weighs more than fat, which explains why athletes often get mislabeled by basic metrics. Bioelectrical impedance scales or DEXA scans provide clearer insights into body composition. The CDC notes these tools help identify sarcopenia—age-related muscle loss affecting mobility.
Healthy body fat ranges vary by age and sex:
- Women: 21-33% (ages 20-59)
- Men: 8-22% (ages 20-59)
Pairing these metrics with traditional measurements creates a holistic health profile. As research confirms, people with normal indexes but high body fat face similar obesity-related risks as those classified overweight.
Insights from Research and Health Authorities
Cutting-edge research reshapes how we interpret health metrics across life stages. Leading institutions like the CDC and NIH continuously refine guidelines to reflect biological diversity and emerging science.
Data from CDC, NIH, and Other Sources
The CDC emphasizes that muscle mass significantly impacts weight classification. Their 2023 report notes athletes often score higher on traditional metrics despite lower body fat—a gap addressed in updated screening tools.
NIH studies reveal sex-specific differences. Women naturally carry more essential fat, yet outdated charts sometimes misclassify their health risks. Revised guidelines now account for hormonal fluctuations and bone density changes with age.
Recent Studies on BMI, Age, and Health Risks
A 2024 Journal of Gerontology study found adults over 65 with slightly elevated scores had lower mortality rates—the “obesity paradox.” Researchers stress pairing metrics with muscle assessments for accurate risk profiles.
Key findings from recent analyses:
| Study Focus | Key Finding | Population |
|---|---|---|
| Muscle vs. Fat | 30% of athletes misclassified | Ages 18-40 |
| Height Variations | Taller individuals show lower cardiac risks | Women 50+ |
| Gender Factors | Waist measurement >35″ doubles diabetes risk | Females 30-60 |
These studies highlight why one-size-fits-all approaches fail. As NIH experts state: “Health evaluations must evolve with demographic and physiological factors to remain relevant.”
BMI Trends in Older Adults: Adjusting for Age and Health
As we age, our bodies rewrite the rules of health—numbers that once signaled risk might now suggest resilience. Recent studies reveal surprising patterns in how weight and health status interact after 65. This shift demands fresh approaches to evaluating disease risks in older populations.
Understanding the Obesity Paradox in Seniors
Research shows seniors with slightly higher weight often outlive thinner peers—a phenomenon called the obesity paradox. A 2023 Journal of Aging Research study found adults over 70 with indexes in the “overweight” range had 20% lower mortality from heart disease. This protective effect stems from extra energy reserves during illness and reduced frailty risks.
Consider these age-specific factors:
- Muscle loss accelerates after 60, making pounds on the scale less reliable
- Waist measurements over 35 inches (women) or 40 inches (men) still indicate elevated risks
- Sex differences matter—women retain more fat for hormonal health
One Harvard study tracked 6,000 seniors for a decade. Those classified as moderately overweight faced fewer hospitalizations than peers in “normal” ranges. However, extreme obesity (risks by 40%.
Health professionals now emphasize personalized health status evaluations over generic charts. As Dr. Linda Mitchell notes: “A 75-year-old with controlled blood pressure and active lifestyle might thrive at weights that concern younger adults.” Context transforms numbers from warnings to wisdom.
Conclusion
Decoding health risks means looking beyond generic numbers to life-stage realities. Age-specific tools like tailored weight-to-height evaluations provide clearer insights than static measurements. Studies from leading health authorities confirm these resources help identify trends when paired with muscle assessments and waist measurements.
Body composition shifts across decades—a fact traditional metrics often miss. Combining index ranges with visceral fat analysis and activity levels creates a fuller picture. The CDC and NIH both recommend this blended approach for accurate risk predictions.
Consistent monitoring matters more than isolated numbers. Regular check-ins with healthcare providers help contextualize results against personal health histories. This proactive strategy turns data into actionable steps for maintaining wellness.
Ultimately, informed decisions come from understanding how age shapes our bodies. Trusted guidelines and professional guidance transform simple measurements into powerful health allies. Embrace tools that grow with you—they’re the key to lifelong vitality.


