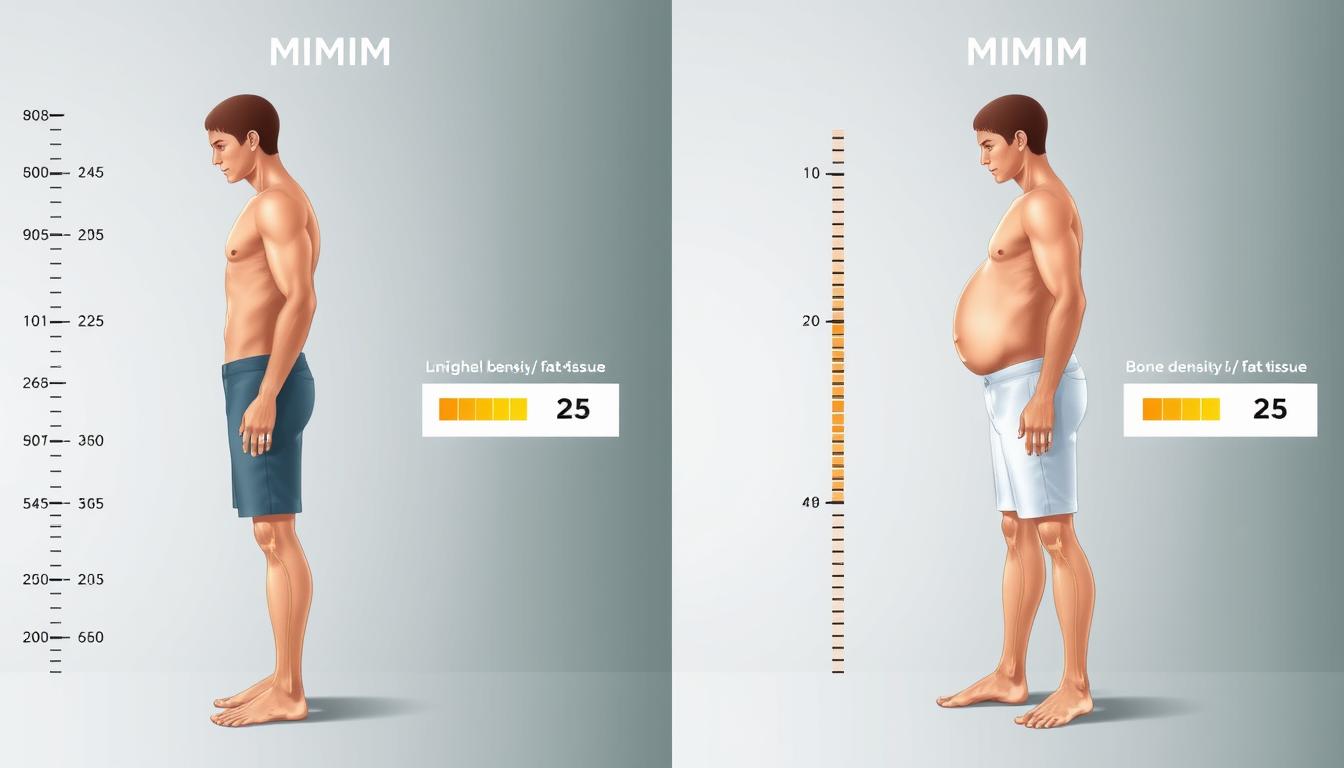
Figure 1: Two individuals with identical BMI but different bone mass and body composition, demonstrating BMI’s limitation in accounting for bone density variations.
Understanding BMI: Formula and Standard Limitations
Body Mass Index is calculated by dividing a person’s weight in kilograms by the square of their height in meters (kg/m²). This simple formula was developed in the 1830s by Belgian mathematician Adolphe Quetelet as a quick way to categorize weight status. According to standard classifications, a BMI below 18.5 is considered underweight, 18.5-24.9 is normal weight, 25-29.9 is overweight, and 30 or above is obese.
While BMI provides a convenient screening tool for population studies, it fails to account for several critical factors that influence body composition and health. The formula treats all body weight equally, making no distinction between muscle, fat, bone, and other tissues that contribute to total body mass.
Figure 2: The BMI formula and classification ranges, which fail to account for variations in bone mass and other body composition factors.
3 Critical Flaws in BMI Calculations
- Bone mass blind spot: BMI doesn’t differentiate between bone density variations, potentially misclassifying individuals with high or low bone mass
- Muscle-to-fat ratio oversight: Athletes with high muscle mass may be incorrectly labeled as overweight or obese
- Age/gender generalization errors: BMI uses the same thresholds regardless of age, gender, or ethnicity, ignoring natural variations in body composition
Understand Your True Body Composition
Discover how your bone density affects your weight assessment and learn which measurement methods provide the most accurate picture of your health.
The BMI Paradox: When Bones Distort the Numbers
Research has consistently shown that bone mineral density (BMD) can significantly impact BMI readings, creating misleading assessments of weight status. According to a study published in the Journal of Orthopaedic Surgery and Research, BMI calculations become less accurate as bone density deviates from average levels, particularly in individuals with very high or very low bone mass.
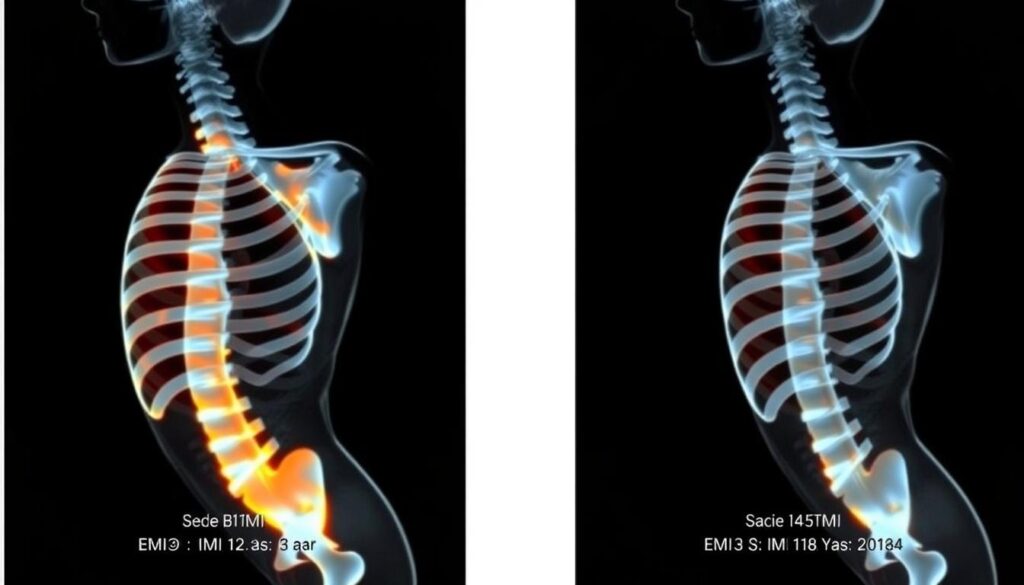
Figure 3: DEXA scan comparison showing significant bone mineral density differences between two individuals with identical BMI measurements.
Bone mass typically accounts for 3-5% of total body weight in healthy adults, but this percentage can vary significantly based on age, gender, genetics, and health conditions. A study conducted by Salamat et al. found that men with higher bone mineral density were often misclassified as overweight based on BMI alone, despite having healthy body fat percentages.
How Bone Density Variations Skew BMI Results
Athletes and individuals who engage in regular weight-bearing exercise typically develop higher bone mineral density as a physiological adaptation. This increased bone mass contributes to their total weight without increasing health risks, yet BMI calculations may incorrectly classify them as overweight.
Conversely, elderly individuals and those with osteoporosis experience bone mineral loss that reduces their total body weight. This can result in a “normal” BMI reading despite potentially unhealthy levels of body fat. According to research by Fawzy et al., BMI was low in 82.4% of people with normal bone mineral density, suggesting that BMI alone is insufficient for assessing body composition in individuals with bone density variations.
“Low BMI is a good indicator for referral of women less than 60 years for measurements of BMD. However, the role of obesity as a risk factor for low BMD, osteoporosis, and its related fractures remains unsettled.”
Key Finding: Research shows that advancing age and lower BMI are important risk factors for the occurrence of low bone mineral density, highlighting the complex relationship between weight, bone mass, and overall health assessment.
| Population Group | Typical Bone Mass Characteristics | Effect on BMI Accuracy | Recommended Assessment |
| Athletes/Weightlifters | Higher bone mineral density | BMI overestimates fat content | DEXA scan, body fat percentage |
| Elderly (65+) | Lower bone mineral density | BMI underestimates fat content | DEXA scan, waist circumference |
| Postmenopausal Women | Accelerated bone loss | BMI may appear normal despite unhealthy body composition | DEXA scan, bioelectrical impedance |
| Individuals with Osteoporosis | Significantly reduced bone mass | BMI significantly underestimates health risks | DEXA scan, comprehensive metabolic assessment |
Real-World Examples: When BMI Gets It Wrong
The Weightlifter’s Dilemma
Consider John, a 45-year-old weightlifter with 15 years of consistent training. At 5’10” (178 cm) and 190 lbs (86 kg), his BMI calculates to 27.3, placing him in the “overweight” category. However, a DEXA scan reveals that John has a bone mineral density 15% above average for his age and a body fat percentage of just 14%, which is considered athletic and healthy.
John’s higher bone mass contributes significantly to his weight without increasing health risks. In fact, his higher bone density provides added protection against fractures and age-related bone loss. Yet, based solely on BMI, John might receive misguided advice to lose weight, which could potentially harm his musculoskeletal health.

Figure 4: A weightlifter with high bone density misclassified as “overweight” by BMI despite healthy body composition.
The Osteoporosis Patient’s False Reassurance
Meanwhile, Margaret, a 72-year-old woman with diagnosed osteoporosis, stands 5’4″ (163 cm) and weighs 130 lbs (59 kg). Her BMI calculates to 22.3, placing her squarely in the “normal weight” category. However, a comprehensive body composition assessment reveals that Margaret has significantly reduced bone mass and a body fat percentage of 34%, which exceeds healthy recommendations for her age.
Margaret’s reduced bone mass masks her unhealthy body fat levels when using BMI alone. Her healthcare provider might miss important interventions for reducing cardiovascular and metabolic risks if relying solely on BMI as an indicator of health status.
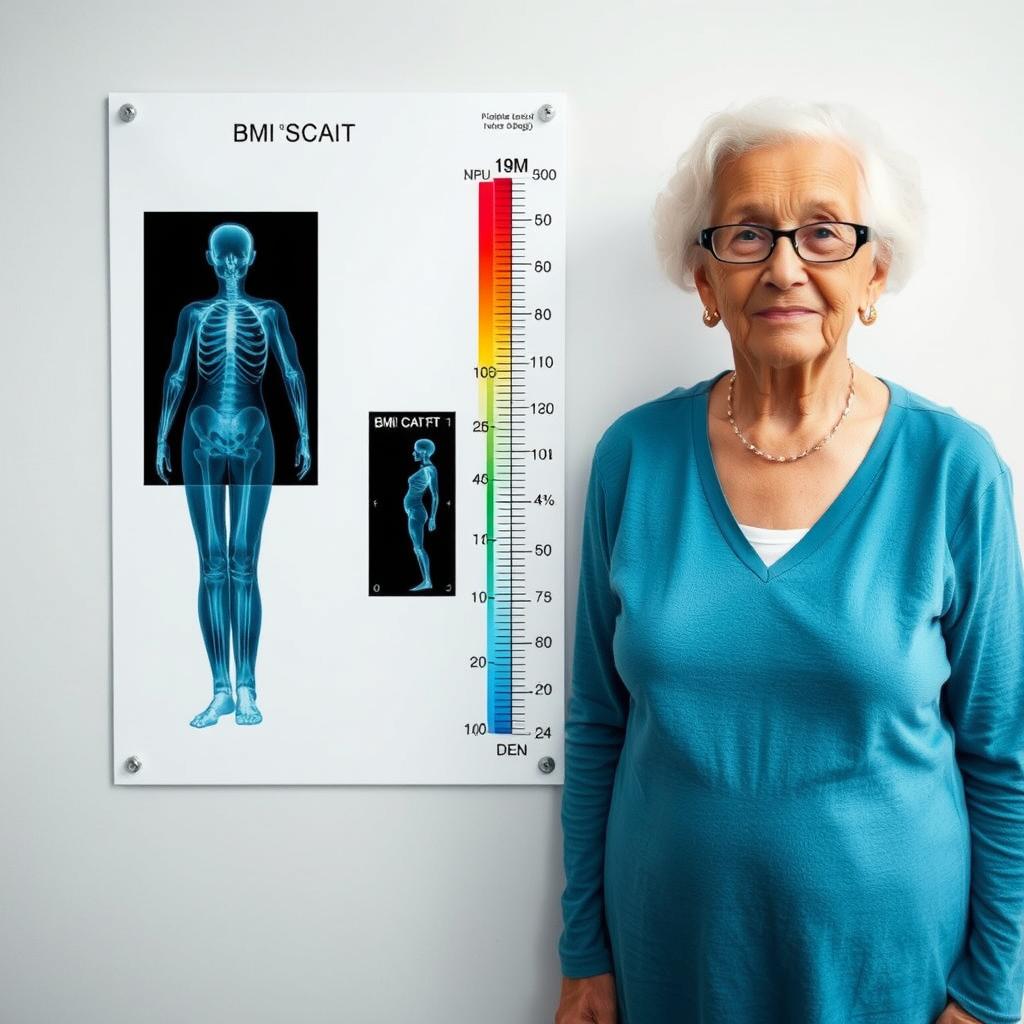
Figure 5: An osteoporosis patient classified as “normal weight” by BMI despite unhealthy body composition.
Beyond BMI: Get the Complete Picture
Learn how to interpret your body composition results and understand what they mean for your long-term health.
Beyond BMI: Comparing Body Composition Analysis Methods
While BMI provides a quick screening tool, more sophisticated methods offer greater accuracy in assessing body composition, particularly for individuals with bone mass variations. Dual-Energy X-Ray Absorptiometry (DEXA) has emerged as the gold standard for measuring bone mineral density and body composition.

Figure 6: DEXA scan procedure providing detailed analysis of bone mineral density, lean mass, and fat mass.
DEXA Scans vs. BMI: The Accuracy Gap
DEXA scans use two different X-ray beams to assess bone density and soft tissue composition throughout the body. Unlike BMI, which treats all weight equally, DEXA distinguishes between bone, fat, and lean tissue, providing a comprehensive picture of body composition.
According to research published in the Journal of Orthopaedic Surgery and Research, DEXA measurements can identify individuals with low bone mineral density who might otherwise be misclassified by BMI alone. This is particularly important for early intervention in conditions like osteoporosis and sarcopenia (age-related muscle loss).
DEXA Scan Advantages
- Distinguishes between bone, fat, and lean tissue
- Provides regional body composition analysis
- Gold standard for bone mineral density measurement
- High precision and reproducibility
- Detects small changes in body composition over time
DEXA Scan Limitations
- Higher cost than simple BMI calculation
- Limited availability outside medical settings
- Requires specialized equipment and trained technicians
- Involves minimal radiation exposure
- May be affected by hydration status
Alternative Body Composition Assessment Methods
| Method | How It Works | Accuracy for Bone Assessment | Accessibility | Cost |
| BMI | Weight (kg) ÷ Height² (m) | Poor – Does not measure bone | Very High | Free |
| DEXA Scan | Dual-energy X-ray beams measure tissue absorption | Excellent – Gold standard | Low – Medical facilities only | $100-300 |
| Bioelectrical Impedance (BIA) | Electrical current measures resistance in tissues | Fair – Estimates only | High – Home devices available | $30-300 |
| Hydrostatic Weighing | Underwater weighing based on displacement | Good – Indirect measurement | Very Low – Specialized labs | $50-100 |
| Skinfold Calipers | Measures subcutaneous fat at multiple sites | Poor – No bone assessment | Medium – Requires training | $5-50 |
| Vertebral Bone Quality (VBQ) | MRI-based assessment of vertebral fat content | Very Good – Specific to spine | Low – Requires MRI | $200-500 |
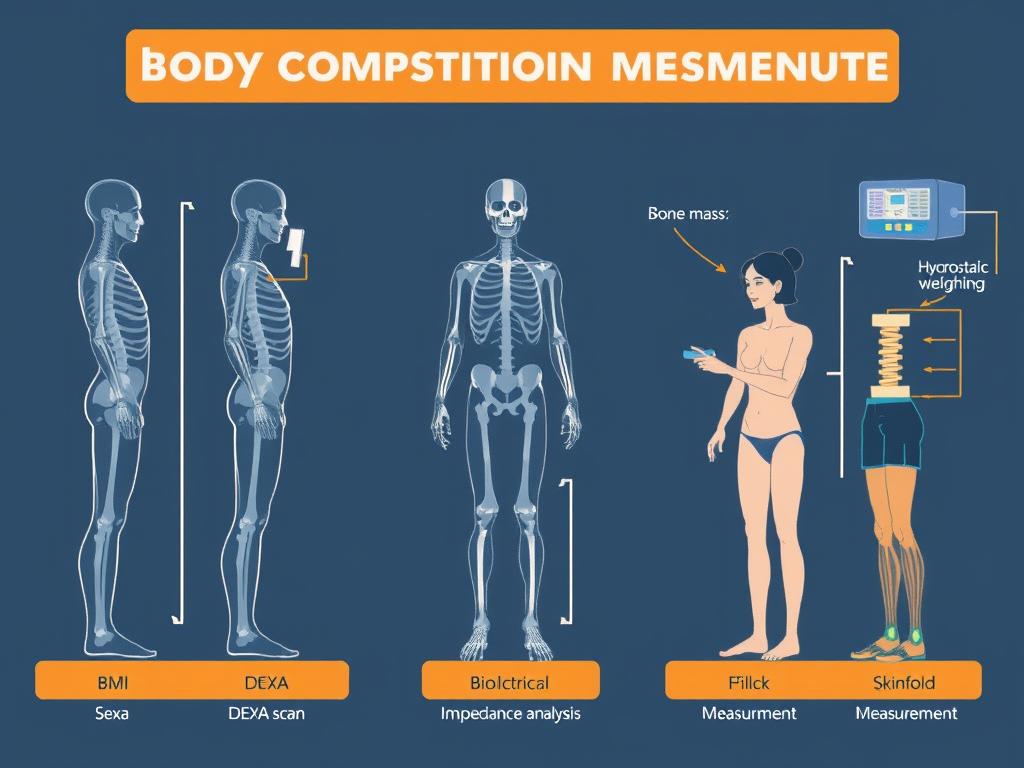
Figure 7: Visual comparison of different body composition assessment methods and their ability to measure bone mass.
Guidance for Healthcare Professionals: Interpreting BMI in High/Low Bone Mass Cases
For healthcare professionals, accurately assessing patients with bone mass variations requires looking beyond BMI to more comprehensive evaluation methods. Research by Wang et al. indicates that sex differences significantly affect the accuracy of bone quality assessments, with correlation between bone quality scores and BMD T-values being higher in female patients than in male patients.
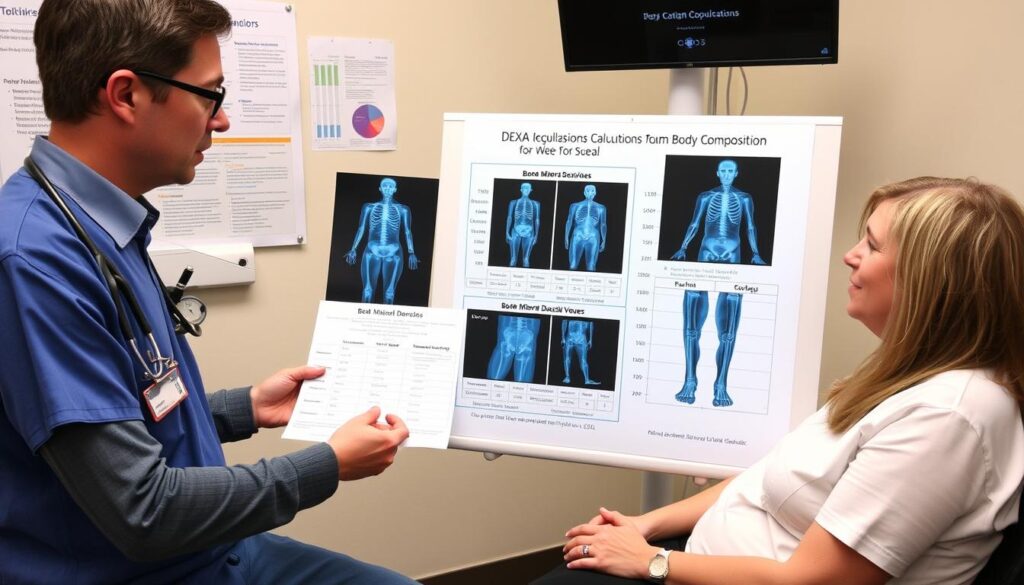
Figure 8: Healthcare professional discussing comprehensive body composition assessment with a patient, moving beyond BMI limitations.
Clinical Assessment Recommendations
For Patients with Suspected High Bone Mass
- Consider athletic history and resistance training background
- Evaluate muscle mass through physical examination and imaging
- Assess cardiovascular fitness independent of BMI classification
- Use waist-to-hip ratio to evaluate fat distribution
- Consider DEXA scan for accurate body composition analysis
For Patients with Suspected Low Bone Mass
- Screen for risk factors including age, menopause status, and medication history
- Evaluate for height loss, which may indicate vertebral compression
- Consider FRAX® tool for fracture risk assessment
- Recommend DEXA scan for definitive diagnosis
- Assess body fat percentage through alternative methods
Clinical Pearl: In patients with BMI
Adjusting BMI Interpretation Based on Bone Health
When DEXA scanning is unavailable, healthcare professionals can use several strategies to improve BMI interpretation:
- Consider age-related bone loss when interpreting BMI in elderly patients
- Evaluate family history of osteoporosis or high bone density
- Assess physical activity patterns, particularly weight-bearing exercise
- Use bioelectrical impedance analysis as a complementary measure
- Consider ethnicity-specific BMI adjustments, as bone density varies across populations
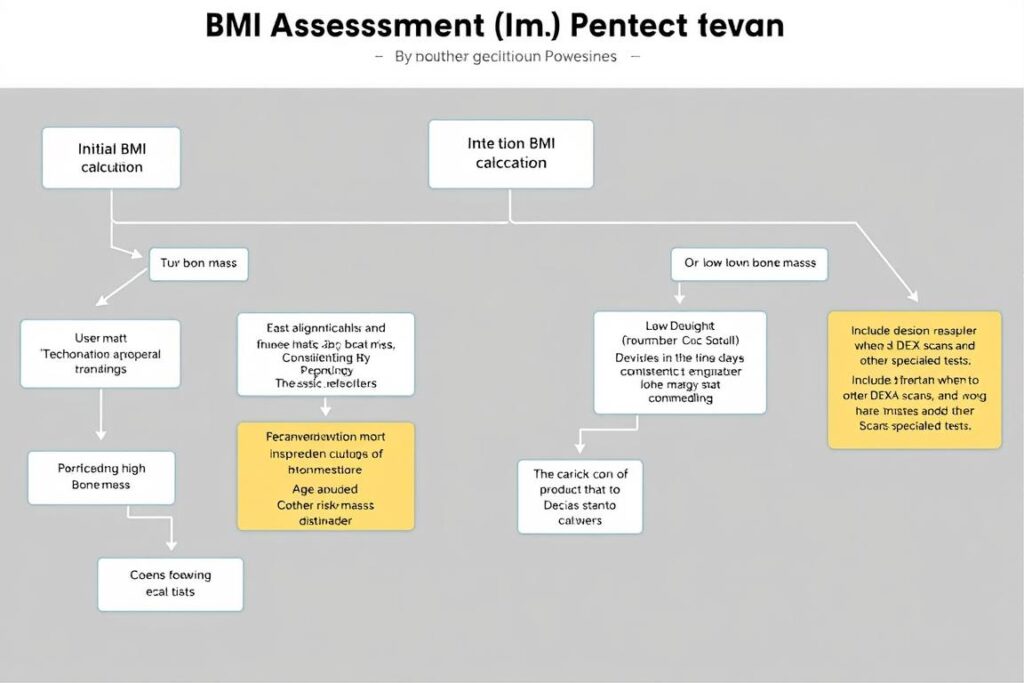
Figure 9: Clinical decision pathway for assessing patients with suspected bone mass variations that may affect BMI interpretation.
Professional Resources for Healthcare Providers
Access evidence-based protocols for accurate body composition assessment in patients with bone mass variations.
Assessing Your Own Body Composition: Beyond the BMI Number
For individuals concerned about the accuracy of their BMI classification, several approaches can provide a more comprehensive understanding of body composition and health status. While professional assessment offers the most accurate results, these self-assessment strategies can help determine whether bone mass might be affecting your BMI reading.

Figure 10: Modern bioelectrical impedance scales provide estimates of bone mass, muscle mass, and body fat percentage for home use.
Self-Assessment Questions to Consider
Do you have a history of resistance training or weight-bearing exercise?
Regular resistance training and weight-bearing exercise stimulate bone growth and increase bone mineral density. If you’ve consistently engaged in these activities for years, your bone mass may be higher than average, potentially affecting your BMI classification.
Are you post-menopausal or over 65 years of age?
Age-related bone loss accelerates after menopause and in later life. If you’re in these demographic groups, your bone mass may be lower than average, potentially masking unhealthy body fat levels despite a “normal” BMI reading.
Have you been diagnosed with osteopenia, osteoporosis, or other bone-related conditions?
These conditions directly affect bone mineral density and total bone mass. If you have a diagnosed bone condition, your BMI may not accurately reflect your body composition or health risks.
Does your BMI classification seem inconsistent with your physical appearance or fitness level?
If you appear lean but have an “overweight” BMI, or appear to carry excess fat despite a “normal” BMI, bone mass variations may be contributing to this discrepancy.
Complementary Measurements to Consider
Waist Circumference
Measure your waist at the narrowest point between the bottom of your ribs and the top of your hips. A waist circumference greater than 35 inches (88 cm) for women or 40 inches (102 cm) for men indicates increased health risk, regardless of BMI.
Waist-to-Hip Ratio
Divide your waist measurement by your hip measurement (taken at the widest part of your buttocks). Ratios above 0.85 for women or 0.90 for men suggest central adiposity and increased health risk.
Body Fat Percentage
Home bioelectrical impedance scales can estimate body fat percentage. While not as accurate as DEXA scans, they provide more information than BMI alone. Healthy ranges vary by age and gender.

Figure 11: Complementary measurements like waist circumference provide additional context for BMI interpretation.
Key Takeaways: Is Your BMI Telling the Truth?
The relationship between bone mass and BMI accuracy is complex and significant. Research consistently shows that BMI calculations can be misleading for individuals with bone mass variations, potentially resulting in inappropriate health recommendations.
For healthcare professionals, recognizing these limitations is crucial for providing accurate patient assessment. Incorporating bone mineral density evaluation, particularly through DEXA scanning when available, offers a more complete picture of body composition and health status.
For individuals, understanding that BMI is merely a starting point rather than a definitive health measure can lead to more informed health decisions. Those with athletic backgrounds, advanced age, or known bone conditions should be particularly cautious about relying solely on BMI for health assessment.
As measurement technology becomes more accessible, we may see a shift away from BMI toward more comprehensive body composition assessment methods. Until then, combining BMI with additional measurements and contextual factors provides the most accurate approach to evaluating weight-related health status.
The science is clear: bone mass matters when interpreting BMI, and a one-size-fits-all approach to weight assessment fails to capture the complexity of human body composition. By understanding these nuances, both healthcare providers and individuals can make more informed decisions about weight management and overall health.
Take Control of Your Body Composition Assessment
Get our comprehensive guide to accurate body composition measurement and learn how to interpret your results based on your unique physical characteristics.