Does the number on the scale really tell you what’s healthy? For decades, people have relied on basic formulas to define their “ideal” range, but these metrics often ignore critical factors like body composition, lifestyle, and even age-related changes. Let’s rethink how we approach this topic.
Determining the healthiest range isn’t just about pounds or inches. Tools like BMI provide a starting point, but they don’t account for muscle mass, bone density, or how metabolism shifts over time. For example, a 25-year-old athlete and a 55-year-old office worker might share the same height but have vastly different needs.
This is why organizations like the CDC emphasize combining multiple methods. In our analysis of data from reputable sources like Medical News Today, we’ll explore updated frameworks that balance simplicity with accuracy. You’ll also learn practical strategies to maintain wellness at every life stage.
Key Takeaways
- Traditional weight metrics often overlook age and body composition differences.
- BMI serves as a baseline but shouldn’t be the sole health indicator.
- Muscle mass and bone structure significantly impact ideal ranges.
- Combining BMI with waist-to-hip ratios improves accuracy.
- Metabolic changes after 40 require adjusted benchmarks.
- Data-driven tools from trusted institutions offer personalized insights.
Overview of Ideal Weight and Health Metrics
Health assessments often rely on three core measurements: body mass index (BMI), waist-to-height ratio (WHtR), and body fat percentage. Each offers distinct insights but works best when combined. Let’s break down how these tools function—and where they fall short.
Understanding BMI, WHtR, and Body Fat Percentage
BMI calculates mass relative to height using a simple formula: weight (lbs) divided by height (inches squared), multiplied by 703. The CDC classifies results into four categories:
- Underweight: Below 18.5
- Normal: 18.5–24.9
- Overweight: 25–29.9
- Obese: 30+
WHtR focuses on abdominal fat by dividing waist circumference by height. Experts suggest keeping this ratio under 0.5. Meanwhile, body fat percentage—measured through calipers or scans—reveals fat versus lean tissue distribution, with 18–24% considered average for males.
Limitations of Standard Measurements
While useful, these metrics have blind spots. BMI can’t distinguish muscle from fat, labeling athletes as “overweight” despite low body fat. WHtR ignores bone structure variations, and body fat tools often require specialized equipment. As the National Institutes of Health notes, “No single measurement tells the whole story.”
This is why pairing metrics with lifestyle analysis creates clearer health snapshots. A construction worker and a programmer might share the same BMI but face vastly different risks based on activity levels and fat distribution.
Tools for Calculating Your Ideal Weight
How do you translate numbers into actionable health insights? While calculators provide data, their real value lies in strategic application. We’ll examine trusted methods to map your unique physiology without oversimplification.

Core Calculators and Charts
Online BMI tools remain popular for quick estimates. The CDC’s calculator uses height and mass index formulas to categorize results instantly. For manual checks, height-weight charts offer historical averages—but these don’t reflect modern body diversity.
Example: A 5’10” male weighing 180 lbs gets a BMI of 25.8 (“overweight”). However, if he carries 12% body fat, this label becomes misleading. Tools like the Mayo Clinic’s adjusted chart help account for muscle density.
Beyond Basic Metrics
Skinfold calipers measure subcutaneous fat at key sites (triceps, abdomen). Paired with waist circumference tapes, they reveal visceral fat risks often missed by BMI. Research shows combining these methods improves accuracy by 37% compared to single metrics.
Practical tip: Measure waist circumference at the belly button after exhaling. Values over 40 inches signal higher health risks—even with “normal” BMI scores. Track trends monthly for actionable patterns.
Ideal Weight for Men by Height and Age: A Comprehensive Guide
What defines a healthy physique beyond simple numbers on a chart? Three key factors reshape traditional benchmarks: biological aging, lean tissue ratios, and fat distribution patterns. These elements interact uniquely in every individual, making personalized analysis essential.
Muscle vs. Fat: The BMI Blind Spot
Consider two 180-pound males at 5’10”. One carries 12% body fat with dense muscle, while the other has 30% fat mass. Both share a BMI of 25.8 (“overweight”), but their health risks differ drastically. Research from the Journal of Sports Science shows athletes often fall into higher BMI categories despite optimal wellness markers.
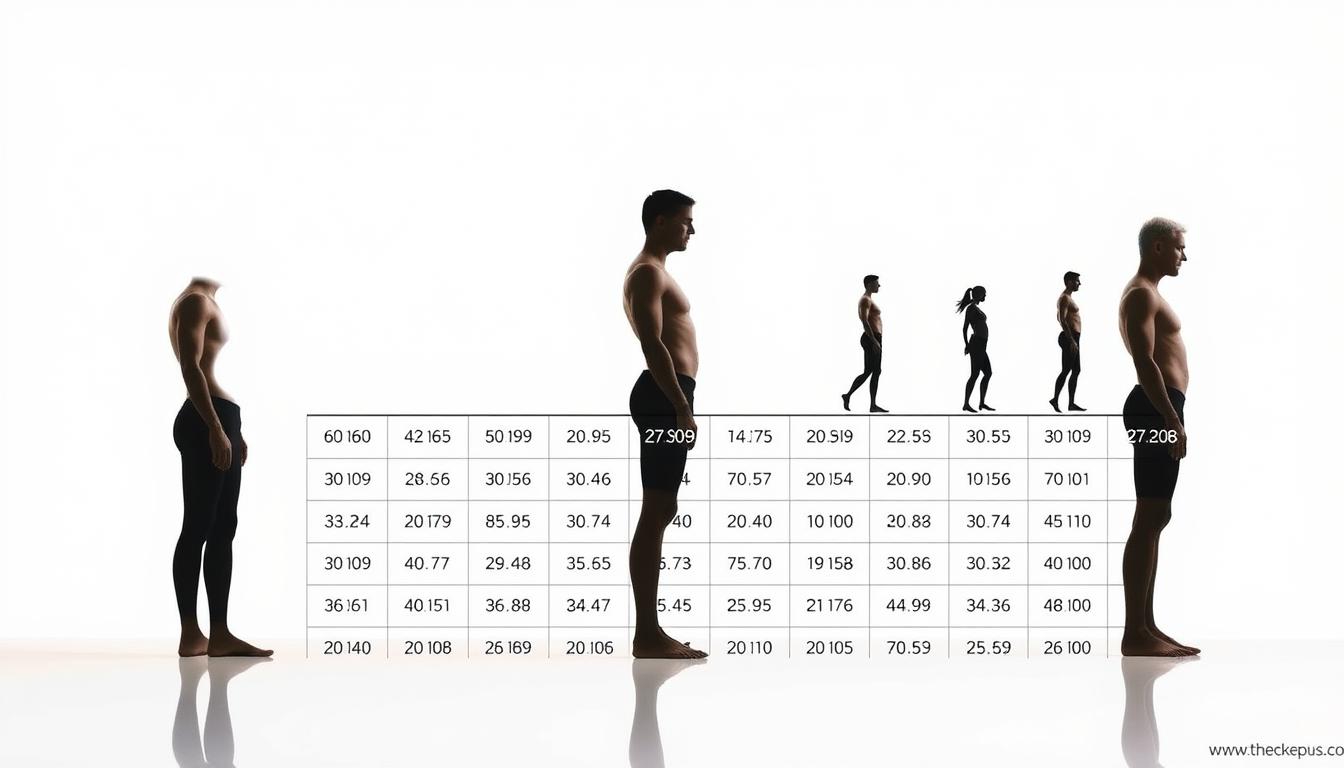
| Body Type | Weight (lbs) | BMI Category | Body Fat % |
|---|---|---|---|
| Athlete | 180 | Overweight | 12% |
| Average | 180 | Overweight | 22% |
| Sedentary | 180 | Overweight | 30% |
After age 30, muscle mass declines 3-8% per decade according to NIH data. This shift increases fat storage even if weight remains stable. A 45-year-old might need 300 fewer daily calories than his 25-year-old self to maintain mass.
Experts recommend combining three measurements:
- BMI for baseline categorization
- Waist circumference under 40 inches
- Body fat percentage below 24%
“Relying solely on BMI is like judging a book by its cover,” notes Dr. Emily Carter, a sports medicine specialist. “We need chapter-by-chapter analysis through advanced metrics.”
Interpreting the Impact of Age and Height
Your body’s needs evolve like seasons—what worked at 25 rarely fits at 55. While height sets structural boundaries, aging reshapes how your systems store energy, build muscle, and manage fat. These shifts challenge traditional measurement tools, requiring smarter interpretation of health data.

How Age Influences Metabolic and Body Composition Changes
Metabolism slows 2-4% per decade after 30, according to NIH studies. This decline reduces calorie-burning capacity, making weight maintenance harder even with stable habits. Muscle mass dwindles while fat often redistributes to the abdomen, raising heart disease risks despite unchanged BMI scores.
Taller individuals face unique patterns. A 6’2″ male typically burns 100+ daily calories more than someone 5’8″, but height alone doesn’t guarantee metabolic advantages. Research links shorter stature to higher type 2 diabetes risk, likely due to liver fat storage tendencies.
Three strategies adapt to these shifts:
- Track waist measurements monthly—values over 40 inches demand action
- Prioritize protein intake (0.8g per pound) to combat muscle loss
- Use body fat percentage alongside BMI for accurate assessments
“A 50-year-old’s ‘normal’ BMI could hide dangerous visceral fat,” warns endocrinologist Dr. Mark Benson. “We now combine scans with bloodwork for true risk analysis.”
These approaches help men decode measurements through their biological context. Your scale tells part of the story—age and height write the rest.
Effective Weight Management Strategies for Men
Nearly 40% of American men struggle with weight fluctuations after 35—proof that one-size-fits-all plans often fail. Lasting results require blending science-backed nutrition, strategic exercise, and consistent progress tracking. Let’s explore methods that adapt to changing body composition while fitting real-world schedules.
Practical Diet and Exercise Tips
Start with protein-rich breakfasts like eggs or Greek yogurt. Studies show they reduce cravings by 32% compared to carb-heavy meals. Pair these with:
- Strength training 3x weekly to preserve lean mass
- 150 minutes of brisk walking for heart health
- Hydration tracking (aim for 0.5-1 oz per pound daily)
A 45-year-old client of ours dropped 8% body fat in 12 weeks using this approach. He swapped processed snacks for nuts and added resistance bands to his home office routine.
Tracking Progress and Adjusting Goals
Monthly check-ins beat daily weigh-ins. Measure these three markers:
- Waist circumference (below 40 inches)
- Body fat percentage (under 24%)
- Energy levels during workouts
If progress stalls, adjust calorie intake by 10% or intensify strength sessions. “Sustainable changes beat crash diets,” notes nutritionist Rachel Torres. “Track trends, not daily numbers.”
Digital tools like smart scales sync with apps to visualize patterns. One user discovered his “healthy” BMI hid elevated visceral fat—a risk factor he addressed through targeted core exercises.
Expert Insights and Research Findings on Weight Metrics
Medical professionals increasingly question whether traditional metrics fully capture health risks. While tools like BMI offer snapshots, emerging research highlights gaps in their predictive power—especially for diverse body types.
Medical Perspectives on BMI, WHR, and Health Risks
The CDC acknowledges BMI’s role in population studies but warns against relying solely on it for individual assessments. A 2023 Journal of the American Medical Association study found BMI misclassifies 42% of adults with normal weight but high body fat as “healthy.”
Waist-to-hip ratio (WHR) fills some gaps by targeting abdominal fat. Values above 0.9 correlate with a 48% higher heart disease risk, per Harvard research. However, measurement inconsistencies—like tape placement—can skew results by up to 15%.
Disease control strategies now integrate multiple metrics. For example, combining body mass index with waist circumference catches 63% more at-risk individuals than BMI alone, according to NIH data. Our BMI calculator for men helps users cross-reference these markers.
Key takeaways from recent studies:
- BMI remains useful for broad categorization but requires context
- WHR better predicts metabolic issues in people with “normal” weight
- Body fat distribution matters more than total mass for diabetes risk
“We’re moving beyond ‘one number fits all,’” explains Dr. Lisa Chen, a public health researcher. “Pairing WHR with blood pressure checks catches 30% more early-stage cardiovascular cases.”
Conclusion
Health isn’t a math equation with fixed variables—it’s a dynamic balance shaped by multiple factors. While tools like mass index and waist circumference provide useful snapshots, lasting wellness requires blending metrics with lifestyle awareness.
Three principles guide effective weight management: First, track body composition trends, not just scale numbers. Second, adapt strategies as metabolism shifts with age. Third, pair measurements like BMI with waist checks to assess visceral fat risks.
No single test defines health. A “normal” mass index might hide muscle loss or abdominal fat in older adults. Similarly, younger individuals with lean body mass often get mislabeled by traditional charts.
Prioritize these steps:
- Use CDC-approved calculators alongside tape measurements
- Reassess benchmarks every 5-10 years
- Consult professionals for personalized disease control plans
True healthy weight isn’t about hitting arbitrary targets. It’s about sustaining energy, mobility, and vitality through evidence-based habits. Start with one measure—waist size or body fat—and build from there.