How do we determine whether a teenager’s weight aligns with their developmental needs? This question sparks vital conversations about body changes during adolescence. Evaluating physical health requires more than numbers – it demands understanding growth patterns, height variations, and individual maturation timelines.
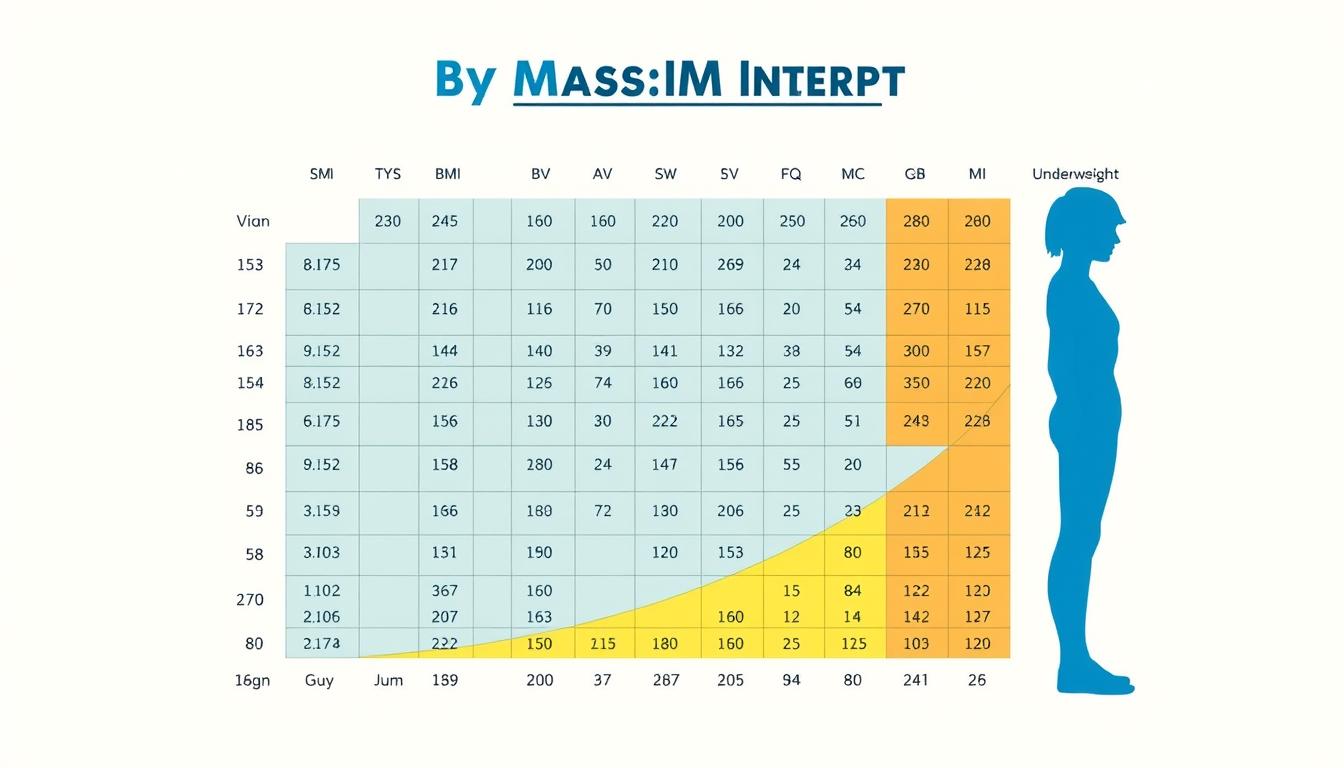
Standard adult BMI calculators often miss critical nuances for developing youth. Tools like the NHS England Child BMI system analyze age-adjusted percentiles, comparing teens to peers rather than adult benchmarks. Growth spurts and hormonal shifts create natural fluctuations that single measurements can’t capture.
We combine quantitative data with qualitative observations to assess wellness. For families and healthcare providers, this means tracking trends over multiple years while considering muscle development and bone structure. Our analysis uses percentile-based charts specifically designed for children and adolescents, ensuring age-appropriate evaluations.
Key Takeaways
- Teen weight assessments require age-specific tools, not adult standards
- Height growth patterns significantly impact weight interpretations
- BMI percentiles compare teens to same-age peers nationwide
- Multiple measurements over time provide clearer health pictures
- Professional guidance ensures accurate developmental evaluations
Understanding Body Mass Index and Healthy Weight Ranges for Teenagers
Evaluating adolescent health requires tools designed for growing bodies. The body mass index (BMI) serves as a starting point for understanding weight-to-height ratios. Unlike adult assessments, youth evaluations must account for rapid physical changes during puberty.
What Is BMI and Its Significance?
BMI calculates body mass using a simple formula: weight in kilograms divided by height in meters squared. While not a direct measure of body fat, it helps identify potential health risks. The CDC states, “BMI percentiles reveal how a teen’s measurements compare to others of the same age and gender.”
BMI Categories and Health Implications for Young People
Standard categories include underweight (below 5th percentile), healthy weight (5th–85th), overweight (85th–95th), and obese (above 95th). However, these ranges don’t tell the full story. Athletic teens with high muscle mass might register higher BMIs without excess fat.
Pediatricians emphasize three critical limitations:
- Doesn’t distinguish between muscle and fat
- Varies by ethnicity and genetic factors
- Requires specialized tools for accurate youth analysis
Using adult BMI calculators for teens leads to flawed conclusions. Instead, CDC growth charts incorporate age-specific percentiles and gender differences. This approach helps families track trends while accounting for natural growth spurts.
Is 70 kg overweight for a 14-year-old?
Assessing adolescent weight involves more than numbers on a scale. Growth patterns and physical maturation create unique combinations that standard metrics often overlook. A teen’s stature and biological timeline dramatically influence what constitutes a healthy measurement.
Evaluating 70 kg in the Context of Age, Height, and Growth
A 14-year-old’s weight becomes meaningful when paired with their height and growth phase. The NHS England Child BMI tool accounts for these variables by comparing measurements to national averages. Growth spurts can temporarily increase weight before height catches up, creating misleading snapshots.

Pediatricians emphasize tracking trends over months rather than single readings. “One measurement tells us little – it’s the trajectory that matters,” notes a Children’s Hospital report. Athletic builds or late bloomers might fall outside standard charts without indicating health risks.
Using BMI Calculators and Tools for Teen Assessments
Specialized BMI calculators for children require precise inputs: birth date, sex, and exact measurements. These tools generate percentile rankings rather than fixed categories. For example, the NHS system flags results above the 85th percentile for further review but considers individual circumstances.
Key steps for accurate analysis:
- Measure height without shoes on a flat surface
- Use calibrated scales for weight checks
- Input data into youth-specific tools
While these calculators provide essential data, they work best alongside professional evaluations. Muscle development and bone density – factors not captured by BMI – complete the health picture.
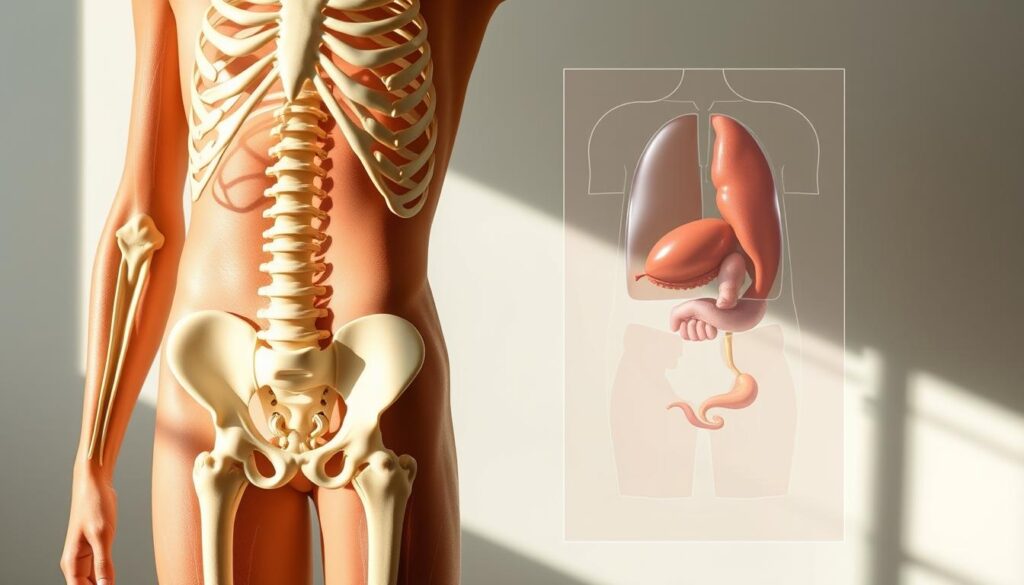
Factors Influencing Teen Weight and Body Composition
Teen weight assessments demand a multidimensional approach that considers biological diversity and lifestyle patterns. While BMI calculators provide foundational insights, they require context from other factors to paint accurate health pictures.
Age, Gender, and Ethnicity in BMI Calculations
Growth timelines vary dramatically across populations. The CDC confirms that ethnicity impacts body fat distribution patterns, with Asian teens often showing higher health risks at lower BMI scores than Caucasian peers. Gender differences emerge during puberty – males typically develop denser muscle mass, while females experience earlier fat redistribution.
Three critical considerations:
- Growth charts differ for athletes versus non-athletes
- Bone density variations affect weight interpretations
- Metabolic conditions like thyroid disorders alter body composition
“Standard BMI categories don’t account for genetic diversity in bone structure or fat storage,” notes a Johns Hopkins pediatric study.
Role of Muscle Mass, Bone Structure, and Lifestyle
Active teens often challenge traditional BMI classifications. A football player might measure 85th percentile body mass due to lean tissue rather than excess fat. DEXA scans reveal some athletes have half the body fat percentage of sedentary peers with identical BMI scores.
Lifestyle elements create further complexity:
- Sleep patterns influence hormonal balance
- Nutrition quality affects fat-to-muscle ratios
- Screen time correlates with visceral fat accumulation
Healthcare providers combine height-weight ratios with skinfold measurements and activity logs for comprehensive evaluations. This layered approach respects individual biology while identifying true health problems.
Conclusion
Understanding adolescent health demands more than isolated numbers. Our analysis confirms that weight evaluations require context – including height, muscle development, and growth patterns. While BMI calculators offer starting points, research from national health studies shows percentile-based assessments better reflect teen biology.
Three critical insights emerge:
- Body composition matters more than scale numbers alone
- Growth charts account for age and gender differences
- Lifestyle changes improve outcomes regardless of initial measurements
Parents and providers should track trends over years, not weeks. Athletic builds or late growth spurts often explain higher weight without indicating obesity. Professional evaluations assess bone density, fat distribution, and metabolic factors that calculators miss.
Prioritize regular check-ups over DIY tools. Small adjustments in nutrition and activity create lasting health benefits. For personalized guidance, consult pediatric specialists who interpret data through developmental lenses.