Have you ever thought if health measurements are fair for everyone? Body Mass Index (BMI) is a common way to check health. But, it can be different for men and women because of body composition.
We use BMI to judge health, but does it really show the whole picture? The answer is in understanding BMI’s details and how it affects different genders.
We will look into BMI and its use, and then into the gender-specific differences that change how we see it.
Key Takeaways
- Understanding BMI and its limitations
- Exploring gender-specific differences in body composition
- The implications of BMI variations by gender
- How health assessments can be made more inclusive
- The importance of considering gender in health evaluations
Understanding Body Mass Index (BMI)
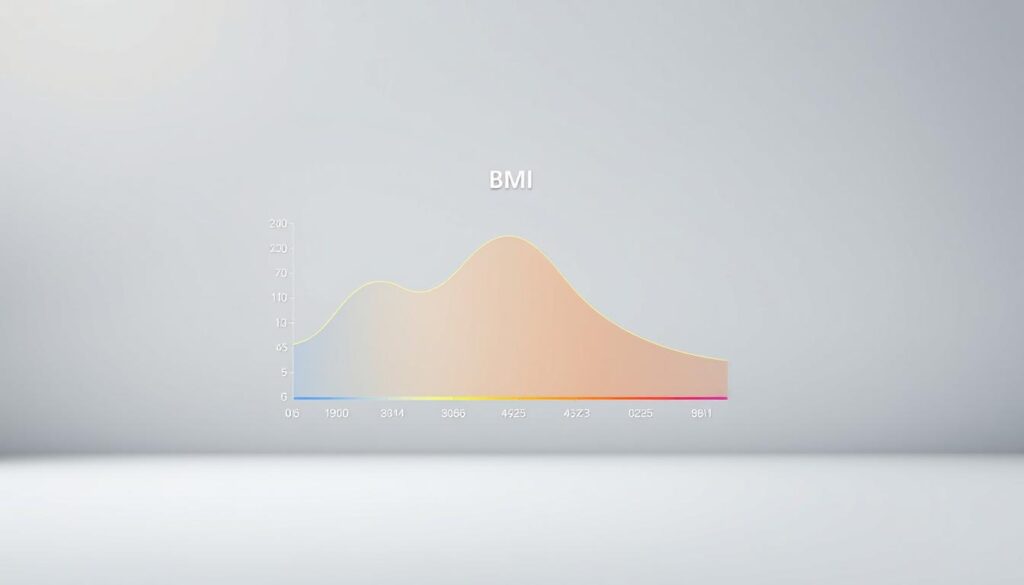
To understand BMI, we first need to know what it measures. Body Mass Index is a simple way to categorize people into different weight groups. These groups include underweight, normal weight, overweight, and obese. It helps us see if our weight is healthy for our height.
What is BMI?
BMI is your weight in kilograms divided by your height in meters squared. It shows if your weight is healthy for your height. It’s a useful tool for both healthcare professionals and individuals to monitor health risks associated with weight.
How is BMI Calculated?
The BMI calculation is easy: divide your weight in kilograms by your height in meters squared (kg/m2). For example, if you weigh 70 kilograms and are 1.75 meters tall, your BMI is 22.86 (70 / (1.75)2). This formula lets us quickly check our weight status.
BMI Categories
The World Health Organization (WHO) has set up several BMI categories. These categories help classify people based on their BMI values. They are:
| BMI Category | BMI Range |
|---|---|
| Underweight | Less than 18.5 |
| Normal weight | 18.5 – 24.9 |
| Overweight | 25 – 29.9 |
| Obese | 30 or greater |
Knowing these categories is key to understanding health risks tied to our weight. For instance, a high BMI can mean a higher risk of heart disease, diabetes, and some cancers.
Biological Differences Between Genders
It’s key to know the biological differences between genders for a better BMI assessment. Men and women have different body compositions and fat distributions. These differences affect how BMI is seen.
Body Composition Variations
Men usually have more muscle and less fat than women. A study on the PMC shows these differences are important for health risks. Since muscle is denser than fat, it changes BMI calculations.
“The gender differences in body composition are significant and should be considered when evaluating an individual’s health risks,” experts say.
Fat Distribution Patterns
Fat distribution varies between genders too. Men often have fat around their belly, called visceral fat. Women usually have fat around their hips and thighs. This is important because visceral fat is linked to higher health risks.
- Men: Higher risk due to visceral fat around the abdomen.
- Women: Fat distribution around hips and thighs, generally considered less risky.
These differences show we need a detailed look at BMI and its health implications. By understanding these biological differences, we can better assess health risks. This helps in creating more effective health strategies.
The Impact of Age on BMI
As we age, our bodies change in ways that affect our Body Mass Index (BMI). It’s important to understand these changes to accurately read BMI at different ages.
One big factor is the loss of muscle mass with age. This is called sarcopenia. Since muscle is denser than fat, losing muscle can lower BMI.
Age-Related Changes in Muscle Mass
Older people often lose muscle mass over time. This can start in the 40s and get worse. Losing muscle can make BMI seem lower, even if fat percentage stays the same or goes up.
- Less physical activity leads to muscle loss.
- Hormonal changes, like lower testosterone, also play a role.
- Eating enough protein is key to keeping muscle.
How Age Affects Body Fat Percentage
With age, where fat is stored changes too. Older adults often gain more fat, mainly around the belly. This can raise BMI, even if weight doesn’t change much.
Some important points to remember:
- Fat moves from outer to inner body parts.
- Metabolism slows down, leading to more fat.
- Less activity and diet changes also affect fat.
It’s crucial to understand these changes to better interpret BMI. For both men and women, these changes can show a contrast in BMI that doesn’t always reflect health. Knowing these gender-specific body mass index distinctions helps give better health advice.
Gender-Specific Health Risks
Gender affects health risks tied to BMI. Men and women face unique challenges based on their BMI.
Studies show that men with a higher BMI are at a higher risk of heart disease. This is due to higher blood pressure and cholesterol levels linked to more body mass.
Men: Higher Risk of Heart Disease
Men tend to store fat around their belly. This fat is linked to heart disease. Visceral fat around organs can cause inflammation and increase heart disease risk.
- Higher blood pressure
- Increased cholesterol levels
- Greater risk of developing type 2 diabetes
For men, a healthy BMI through diet and exercise can lower heart disease risk. Use our BMI calculator to check your BMI and understand your risk better.
Women: Risk of Osteoporosis
Women, mainly after menopause, face a higher risk of osteoporosis with an unhealthy BMI. Both very low and very high BMIs can harm, as they may signal lower bone density or more body fat.
- Post-menopausal women are at higher risk due to decreased estrogen levels.
- Lower body mass can result in less body fat, leading to reduced estrogen levels, further increasing the risk of osteoporosis.
Women can lower this risk by ensuring enough calcium and vitamin D and doing weight-bearing exercises. Monitoring BMI and taking preventive steps can help keep bones healthy.
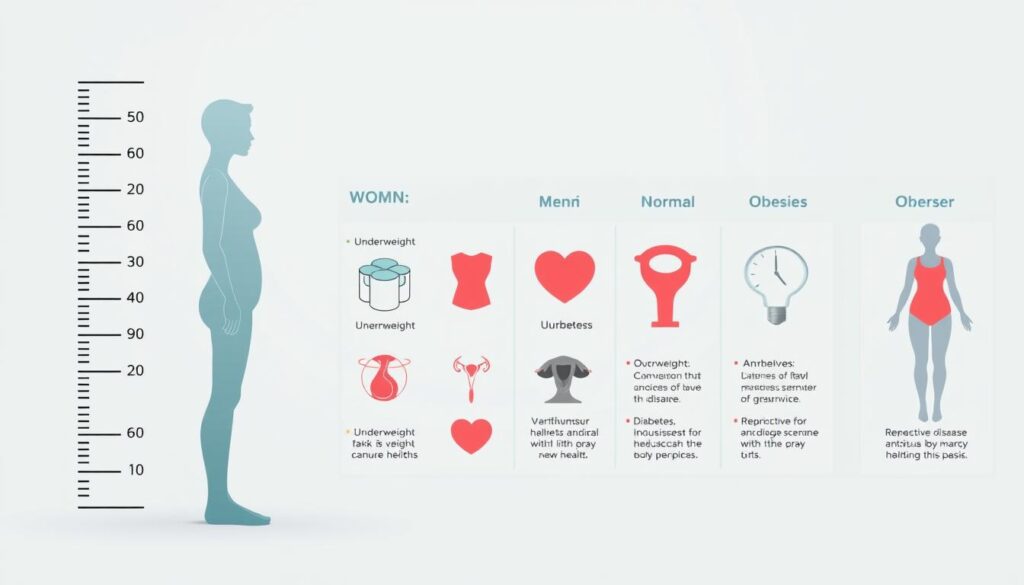
Knowing these gender-specific health risks tied to BMI can help people take steps towards a healthier life. By understanding the risks and taking preventive actions, both men and women can lower their chances of serious health issues.
Limitations of BMI as a Health Metric
BMI is not perfect for measuring health. It doesn’t account for important factors like muscle and body fat. This can lead to wrong classifications, like for athletes or those who are very muscular.
BMI also doesn’t look at where body fat is stored. Visceral fat, around the belly, is riskier than fat in other places.
Does BMI Consider Muscle Mass?
BMI doesn’t tell the difference between muscle and fat. This can make athletes or very muscular people seem overweight or obese. For example, a bodybuilder might have a high BMI but not be overfat.
Table: Comparison of BMI and Body Fat Percentage
| Category | BMI Range | Body Fat Percentage (Men) | Body Fat Percentage (Women) |
|---|---|---|---|
| Underweight | <18.5 | <6% | <16% |
| Normal | 18.5-24.9 | 6-13% | 16-23% |
| Overweight | 25-29.9 | 14-17% | 24-30% |
| Obese | >30 | >17% | >30% |
Cultural and Ethnic Variations in BMI
BMI might not show health risks the same way for everyone. For example, people of Asian descent might have more body fat for the same BMI as Europeans. This means BMI categories might not fit all groups equally.
It’s important to know these limitations for a better health assessment. Healthcare workers should think about these points when using BMI.
Alternative Measures to Consider
Exploring body composition reveals the importance of waist-to-hip ratio and body fat percentage. These metrics offer a detailed look at health risks tied to body composition. They are crucial, given gender influences on BMI calculation.
Waist-to-Hip Ratio
The waist-to-hip ratio is a key indicator of health risks tied to body fat distribution. It’s found by dividing waist circumference by hip circumference. Studies show a higher ratio increases the risk of heart disease and diabetes.
For example, a study found that a higher waist-to-hip ratio in both men and women raises cardiovascular disease risk. This metric is useful for those with a normal BMI but high visceral fat.
Body Fat Percentage
Body fat percentage measures body fat compared to lean body mass. Unlike BMI, it accurately shows health risks from excess fat. It’s a better indicator than BMI for assessing health risks.
For instance, athletes with high muscle mass might have a high BMI but not be overfat. Body fat percentage accurately reflects their health. Recent studies suggest combining BMI with body fat percentage for a full health assessment.
| Health Metric | Description | Health Risk Indicator |
|---|---|---|
| BMI | General measure of body mass relative to height | Potential health risks associated with underweight, overweight, or obesity |
| Waist-to-Hip Ratio | Measure of body fat distribution | Risk of chronic diseases like heart disease and diabetes |
| Body Fat Percentage | Measure of body fat relative to lean body mass | Health risks associated with excess body fat |
Healthcare professionals can better understand an individual’s health by using these measures. This approach helps tailor interventions and grasp the unique health challenges faced by different people.
How to Use BMI Effectively
Knowing if BMI is different for men and women is key to understanding health risks. This article has looked into BMI’s details, including how it varies by gender. It also talked about BMI’s limits as a health measure.
To use BMI well, think about your age, gender, and body type. Doctors can give advice on BMI and other health signs. They consider these factors for you.
Consulting Healthcare Professionals
Talking to doctors can help you understand your health better. They can help you make a plan for a healthy weight and body shape. This approach can lower health risks linked to BMI.


